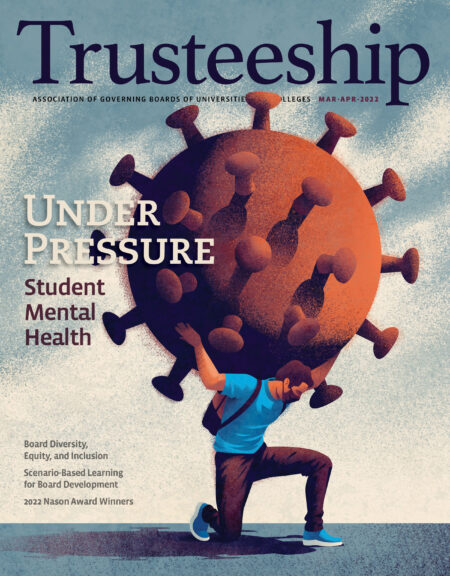
- The coronavirus has taken a significant toll on the mental health of students, exacerbating a crisis that had begun well before the pandemic. There are several reasons for the surge in demand over the last decade, including the fact that seeking mental health services has much less stigma than it used to, but young people are changing too.
- Last spring as campuses pivoted to remote learning, 60 percent of students indicated that the pandemic has made it more difficult to access mental health care. Relative to fall 2019, students reported greater rates of depression compared to spring 2020, according to Healthy Minds. In March through May 2020, a higher proportion of students also reported that their mental health negatively impacted their academic performance.
- One of the by-products of the shift to remote campus services has been a rapid evolution of the delivery of mental health services as campuses invested in training and technology. Teletherapy requires both HIPPA-compliant technology to protect patient’s privacy and staff trained in providing virtual services. Another challenge that counseling centers faced last spring during the transition to remote learning was the licensing of mental health professionals across state lines.
- Several state university and college systems have ramped up investments in mental health this fall, in some cases leveraging the federal COVID-19 relief dollars. The one-time federal funding is in addition to $35 million in investments by campuses, which brings the total financial support in mental health resources to $59 million for the 2021–2022 academic year.
- Colleges could proactively reach out to incoming students to let them know that if they need ongoing therapy—investing in student mental health is good for both students and colleges.
A Spring 2021 survey of college presidents by the American Council on Education showed that senior leaders saw student mental health as the most pressing issue facing their campuses. More than 70 percent of all presidents identified student mental health as an important issue, up from 68 percent in November 2020. The second most commonly selected issue was the mental health of faculty and staff.
“I found it encouraging that…college presidents are showing that student mental health has been a top concern through every stage of the pandemic,” says Sara Abelson, a PhD candidate in public health at the University of Michigan.
It’s important that presidents and boards understand “the importance of making investments not just in mental health intervention but also in promotion and prevention, and especially making investments right now to address issues of equity,” says Abelson, who is also the coinvestigator and lead for diversity, equity, and inclusion projects with the Healthy Minds Network, an interdisciplinary research team focused on adolescent and young adult mental health.
The coronavirus has taken a significant toll on the mental health of students, exacerbating a crisis that had begun well before the pandemic. “There’s really been a rising prevalence of concern for more than a decade at colleges and universities,” Abelson explains. “There’s evidence that the pandemic has added stressors and exacerbated burdens to student and young adult mental health, and we have certainly seen that the pandemic has exacerbated inequities.”
There are several reasons for the surge in demand over the last decade, including the fact that seeking mental health services has much less stigma than it used to, but young people are changing too.
David Reetz, director of counseling and psychological services at Rochester Institute of Technology (RIT), says that the amount of out-of-school social interaction that high school students have with their peers, including participation in athletics, has decreased significantly over the last several years.
“There was this clear socialization trend happening where children and adolescents were spending less and less time with their friends, dating, being involved in part-time work, spending time in communities of faith,” he says.
As a result, young people don’t have as many opportunities to learn how to regulate their emotions or navigate complex social situations—both things new college students are expected to do. “Students coming to college have less and less experience with those things,” he says. “They’re put into this social context, and we see increasing anxiety, year after year…The pandemic has just accelerated that even further with greater social isolation.”
According to a study from EAB, the demand for counseling services was five times greater than enrollment growth between 2009 and 2015. “We know that the demand for mental health services on college campuses has exponentially increased over the last decade, far outpacing the rate of enrollment changes at these universities,” says Brett Scofield, executive director of the Center for Collegiate Mental Health (CCMH) at Pennsylvania State University.
Ninety-four percent of students said that COVID-19 had negatively impacted at least one area of their lives, according to a survey from CCMH of students who were seeking mental health treatment. Seventy-two percent said that the pandemic impacted their mental health, followed by motivation or focus (68 percent), loneliness or isolation (67 percent), academics (66 percent), and missed experiences or opportunities (60 percent). The CCMH surveys focus on students who are seeking treatment from their college counseling centers.
A Healthy Minds study, which samples the entire student population, from March to May 2020 found that “financial stress, a known predictor of student mental health, has been significantly affected by the pandemic: two-thirds of students report their financial situation has become more stressful.”
Last spring as campuses pivoted to remote learning, 60 percent of students indicated that the pandemic has made it more difficult to access mental health care. Relative to fall 2019, students reported greater rates of depression compared to spring 2020, according to Healthy Minds. In March through May 2020, a higher proportion of students also reported that their mental health negatively impacted their academic performance.
Experts say that although students’ utilization of mental health services has decreased since the height of the pandemic, demand may grow this fall as students return to campus. The annual Beginning College Survey of Student Engagement, for example, found that more than half of first-year students starting in fall 2021 reported a substantial increase in mental and emotional exhaustion. In addition, students also reported increased depression, loneliness, and hopelessness.
Sherry Benton, professor emeritus and former director of the counseling and wellness center at the University of Florida, says that an uptick in demand for counseling services several months after a traumatic event is not unusual. “What happens is that in the immediate crisis, you’re in too much shock and just dealing with putting one foot in front of the other to get through it,” she says. “And then afterwards, you’re ready to recognize the impact it had on you and address that.”
While many students reported facing challenges in accessing mental health services at the beginning of the pandemic as colleges scrambled to figure out how to respond, “there’s certainly evidence that schools did a pretty remarkable job quickly pivoting to being able to offer students teletherapy as many institutions first moved to remote learning,” Abelson says.
Questions for Campus Leaders
Boards can ask campus leaders at their institutions these questions to find out how well student mental health needs are being met:
- Who is using your campus counseling center?
- What are the barriers for students who want to use those services?
- Does the makeup of the counselors in your counseling center represent the makeup of your student body?
- Are your institutional policies set up to protect and create safe spaces and belonging for all students at your institution?
- What services does your counseling center provide? What services doesn’t your counseling service provide?
- If you have counselors, what is their clinical load? What experience do you want students to have when they receive treatment at our counseling center?
One of the by-products of the shift to remote campus services has been a rapid evolution of the delivery of mental health services as campuses invested in training and technology. Teletherapy requires both HIPAA-compliant technology to protect patient’s privacy and staff trained in providing virtual services.
“We saw this transformation in mental health service and health-care delivery across the country where virtual services were pretty limited before, basically because of cost and skill,” Reetz of RIT says.
Because of free trainings offered by industry associations, his staff of 20 clinicians were all trained in telemental health at no cost to the institution. Companies such as Zoom also created easy-to-navigate platforms such as Zoom for Healthcare.
Another challenge that counseling centers faced last spring during the transition to remote learning was the licensing of mental health professionals across state lines. Benton, who is also the founder and chief science officer of TAO Connect, says that states have jurisdiction over healthcare regulations, which generally prohibit providers from offering therapy to patients in other states in nonemergency situations. That meant that counselors couldn’t work with out-of-state students.
Benton says that some states loosened licensing requirements for fields like mental health and nursing over the course of the pandemic. “In the past, you could not go across state lines to practice in any way. You had to practice within the state in which you were licensed,” she says. “Some of that has changed.”
She points to the Psychology Interjurisdictional Compact, known as PSYPACT, which allows providers to provide services in any of the states in the compact. As of the end of October 2021, 23 states were participating in the compact, with at least 11 having joined since the start of the pandemic. Another four states are in the process of joining in the next several months, with legislation pending in Wisconsin and Massachusetts.
While experts agree that some form of behavioral telehealth is here to stay, they don’t anticipate that it will ever replace face-to- face services—something that many students are eager for after a year of remote learning. “Telehealth can improve access and convenience for some students, but there’s a lot of students who still prefer in-person services,” Scofield says.
He expects to see more campuses offering hybrid services that “allow for maximum flexibility, where a student could be seen in person as well as remotely depending on student need, staff need, etc.”
Reetz adds that the widespread adoption of teletherapy has increased access. “Developing virtual services really has been a benefit for those students who historically have had a hard time meeting face to face, like the pre-pandemic distance learning students, students who were on internship or co-ops, some graduate students who are only on campus at odd hours, and they’re working full time during the day,” he says. “Now they can know they can have a virtual appointment during their lunch hour.”
The federal government has acknowledged the pressing mental health needs facing both the K–12 and higher education systems. At the end of October, the Department of Education published a new report focused on students’ mental health, Supporting Child and Student Social, Emotional, Behavioral and Mental Health. The report includes several recommendations such as enhancing mental health literacy, using data-driven decision making “to promote equitable implementation and outcomes,” and leveraging policy and funding to bolster mental health support. Mental health is one of the areas in which institutions may utilize the $76 billion from three rounds of federal pandemic relief, known as the Higher Education Emergency Relief Fund (HEERF).
Several state university and college systems have ramped up investments in mental health this fall, in some cases leveraging the federal COVID-19 relief dollars. Chancellor Jim Malatras has directed all colleges and universities in the State University of New York (SUNY) system to spend 5 percent of their institutional grants—$24 million of approximately $481 million systemwide— on student mental health services. The funding will help expand programs such as training additional staff working to residence halls to aid in identifying warning signs and how to refer students to services; expanding SUNY’s Crisis Text Line, peer-to-peer hotlines, and campus student counseling networks.
The one-time federal funding is in addition to $35 million in investments by campuses, which brings the total financial support in mental health resources to $59 million for the 2021–2022 academic year.
According to system officials, the allocation marks the largest single concerted investment in student mental health services in SUNY history. “Our students are dealing with a once in a lifetime health crisis— first from the fear of the unknown and being away from family and friends, and now as we readjust to being in-person again—and coupled with the normal pressures of college, it is affecting their well-being at a higher rate,” Malatras said in a statement. “We can’t expect students to thrive if we can’t be there for them in their time of need. Our students are demanding additional services and we hear them.”
North Carolina is investing $1 million in launching a state-wide initiative that will provide mental health first aid training to staff, students, faculty, and campus police who work for the state university and community college systems as well as independent colleges that participate in the state’s need-based scholarship program. Officials expect more than 10,000 people to participate in the three-day training. Mental health first aid is designed to help individuals who do not have a professional background in mental health recognize the signs of an emerging issue and provide effective, early support to students or colleagues.
The Connecticut State Colleges and Universities (CSCU) system has invested almost $670,000 of COVID-19 relief funding on a two-year contract with telehealth company TimelyMD. System officials said in a statement that every community college student in Connecticut is entitled to free, unlimited access to TalkNow, an on-demand mental health support system, unlimited health consultations, as well as 12 scheduled individual counseling sessions per year.
But the investment has received some pushback from mental health professionals, according to the Connecticut Post. They argued that some of the state’s 12 community colleges don’t have any mental health professionals at all, and that telehealth can’t replace in-person support.
Other state community college systems are also investing in mental health teleservices, in addition to hiring more counselors.
Abelson says that community colleges are more likely to be under resourced in terms of addressing student mental health compared to four-year institutions. “They’re less likely to have psychiatrists available to students and have far fewer providers than four-year institutions,” she says.
Questions for the Board about Student Mental Health
If your board is struggling with how best to respond to the needs and concerns of students—particularly the mental health challenges they present—the following list of questions is a good place to start assessing where your knowledge gaps might lie. The board should also consider periodically inviting the director of the institution’s counseling center to meetings to provide updates on the center’s functioning and to “take the temperature” of the student body.
- Is your board familiar with the requirements of the Family Educational Rights and Privacy Act (FERPA) and the Americans with Disabilities Act (ADA) and confident that the institution is in compliance with them?
- Is your board knowledgeable about the budgetary and staffing needs of the campus counseling center?
- Does your institution have a crisis communications plan in place in the event of an emergency caused by a student suffering from mental health issues?
- Is the director of the institution’s counseling center a licensed professional actively involved in his or her professional association(s) and current on emerging case law and evolving best practices?
- Are there memoranda of understanding in place for relationships with local emergency rooms, crisis centers, and counseling practices that make clear how information will (or will not) be shared?
- Are service limitations (session limits, after-hours access, medication provider availability) clearly indicated on the institution’s website where a prospective student and family can easily find them?
- Are admissions staff knowledgeable about services (and limitations), and aware of relevant staff and how to refer families to them?
- If the institution provides access to a tuition insurance plan, is mental health covered in the event a student needs to leave mid-semester? Does the health insurance plan recommended by the institution also cover mental health conditions adequately?
- Is the institution employing a range of harm-reduction approaches, including peer education, to address issues such as binge drinking, suicide, and illicit and prescription drug use/abuse?
- Are measures for academic and social performance included in the institution’s metrics for identifying and assisting students most at risk of dropping out or needing additional services? This should be part of the institution’s retention efforts for at-risk students.
–Lee Burdette Williams, PhD, is the senior director for mental health initiatives at the National Association of Student Personnel Administrators. This information was included in her article, “Under Pressure: The Growing Demand for Student Mental Health Services” in the May/June 2017 issue of Trusteeship magazine.
“One of the most important things for campus leaders to know is that student mental health is essential for their other institutional goals and priorities,” Abelson says. “There is a huge need to be addressing mental health from a public health perspective and there’s a tremendous opportunity to be focusing on mental health prevention and promotion, not just intervention.”
Focusing on prevention can be an important way to keep students from reaching a mental health crisis in the first place. “There’s a lot we can all be doing to be sort of addressing students who may be at risk or may be showing early signs and intervening to sort of prevent the longer-term development of disorders or suicide,” Abelson says. “And then for those students who do have a mental health disorder, evidence is certainly strongest about [the effectiveness of ] clinical services and treatment.”
She says that since the beginning of the pandemic, colleges and universities have been inundated with companies offering mental health, mindfulness, and meditation apps. She says there is some evidence about the value of those approaches, but there’s not currently a lot of data about which ones are most effective for which types of students as well as how long students need to participate to benefit. But there is some evidence that peer-to-peer programs and mindfulness activities can be beneficial to students, she adds.
When it comes to apps, college officials want to look at utilization and drop-off rates to see whether and how students are using the services, Reetz says.
Scofield says that institutions are offering several options to support students’ mental health, ranging from individual and group therapy to wellness platforms that provide self-guided programs to help students manage stress.
Reetz says that what is needed is for the entire university to think about how the entire learning environment might have a positive impact on students’ mental health. “We want to creatively reshape our learning environments to increase student help-seeking behavior,” he says.
Not only should administrators offer more mental health-related training to faculty, they also need to give faculty the time to take the training. “I can’t tell a faculty member what to do with their schedule in their classroom; they’re going to need support and guidance from academic affairs and the provost’s office,” he says. “The faculty need that time carved out for them.”
Reetz has been studying how universities can encourage students to seek help when they need it in hopes of reducing the number of students who reach a crisis point. The counseling center at RIT started working with a group of five faculty members who added a statement in their syllabus acknowledging that students might face challenges and inviting them to ask for help. The professors explicitly discussed the statement on the first day of class.
The counseling center administered surveys 6 and 12 weeks later and 95 percent reported remembering the syllabus statement because the professor talked about it. More than three quarters of students said that they felt more comfortable asking for help and speaking with their professors about difficult topics.
Reetz says that there’s a common idea among counseling center staff that it’s not possible for colleges to hire their way out of the student mental health crisis. Several studies have shown that counseling centers that hire new staff quickly see their appointments book up without reducing waiting lists.
While that argument has some merit, he says, it doesn’t acknowledge the role that counseling centers can play in serving the larger campus community. “The more you invest in mental health services or staff, there’s a whole lot more that you can do,” he says. “The larger your team is, the more campuswide trainings you can do because direct clinical service isn’t the only thing that we do; we’re serving the entire community. That’s how we’re meeting the mission of higher education.”
He adds that it’s also important for wellness and counseling centers to be upfront about what services they can and cannot provide. “The scope of practice, as we say, should be made very clear,” he says.
Colleges could proactively reach out to incoming students to let them know that if they need ongoing therapy, they might want to start reaching out to community providers. “There’s that upfront planning that we’re trying to do that reduces some of the bottle-necking traffic,” Reetz says. “Colleges and universities aren’t comprehensive healthcare facilities. There’s some things we can do, but we can’t provide everything to all students.”
Scofield underscores that point. “Be transparent with your stakeholders about what the staffing of your counseling center is and what they can realistically do because the lack of alignment of what is the reality on the ground that the counseling center can provide and what stakeholders expect can cause counseling centers to be under fire,” he says.
Abelson says that investing in student mental health is good for both students and colleges. “At a time when so many of our colleges are paying attention to retention and graduation rates, and knowing we need to do better in addressing issues of equity in those arenas, addressing student mental health is essential,” she says. “We have data from the Healthy Minds Network demonstrating that it’s in the best interest of the institution’s bottom line, and that there’s huge return on investment for making investments in mental health.”
Charlotte West is a freelance education reporter. Her work has appeared in the Hechinger Report, USA Today, the Washington Post, and International Educator, among others.
Liability and Risk
How does this impact governance and the responsibilities of governing boards?
Institutions are facing a growing wave of need and demand for mental health services. Counseling centers are admirably stacking sandbags against that rising water, but as those responsible for an institution’s fiscal health, trustees know that there must be a limit to those sandbags.
One answer, to extend the metaphor, is to go “upstream” to the earliest interactions with prospective students and share with them the limitations of mental health services on campus. Rather than offering the blanket statements that are often made in admissions presentations—“free, unlimited counseling services” or “a psychiatrist on staff” when in reality, it’s an eight-hour-per- week contracted employee—colleges and universities need to talk honestly about service limitations— for example, that a center is only open from 8 a.m. to 6 p.m., and after-hours services are provided by a local agency or hospital emergency room.
Such honest conversations may result in families thinking more carefully about their students’ mental health needs. They may talk with their current providers about continuing care via Skype or phone, for example. They may request that pediatricians who have been prescribing medication for years continue to do so, even if students cannot be seen in the office as frequently. They may look outside the campus community for an appropriate provider and research ways for their students to receive treatment from that person.
The topics of liability and risk are critical in understanding how a college counseling center must structure its staff and response protocols. Counselors and psychiatrists at college counseling centers have found themselves the targets of litigation by students or their families who believed that a counselor provided inadequate treatment and, because of that treatment, harm occurred. A student’s suicide is often at the center of such litigation, although lawsuits resulting from harm caused to others by a mentally ill student are also becoming more commonplace. The 2007 Virginia Tech shooting may be the best-known example. Emerging case law is providing some guidance around the obligations of a counselor’s (and counseling center’s) treatment of a student, but, as is the case with all litigation-based instruction, it is happening slowly. In the meantime, thousands of students are seeking mental health services on their campuses.
Licensed counseling professionals generally have malpractice insurance adequate to support their defense in such a lawsuit, and, of course, colleges and universities carry their own liability insurance to cover such situations. But what may be overlooked in the legal wrangling is the cost of personnel hours and morale when a college counselor is named in a suit. Every hour a counselor must spend attending depositions, assembling records, strategizing with attorneys, or sitting through a trial is an hour that person is not available to work with a student in need. And the stress of being brought before a licensure board is as daunting as a lawsuit.
The threat of litigation becomes a more dire issue with each passing year as the number of students with serious pre-existing mental health conditions arriving on campus increases. While working with students who are struggling with the major life transitions endemic to this phase of life is the reason college counseling centers were developed in the first place, our campuses are seeing more and more students with not just serious mood and anxiety disorders but severe eating disorders and longstanding substance abuse issues, as well. In fact, the number of students coming to college in recovery from a serious drug or alcohol addiction is growing rapidly enough that “recovery housing” is becoming common on larger campuses. The state of New Jersey recently passed legislation requiring that state schools provide students with a sober housing option—an admirable idea, but one that brings with it more liability concerns.
The support provided by sober housing is intuitively recognized by anyone who has worked with students in any kind of support groups. Living with, and interacting with, students who share one’s challenges can be helpful. It is not hard, then, to imagine demands for housing that supports students with other mental and emotional health conditions. Clinically, this is an intriguing idea. From a resource perspective (primarily staffing), it is challenging. And from a risk perspective, it raises the question of an institution’s liability for admitting and promising support to a student with a known history of mental illness.
This should not be interpreted as a suggestion that colleges and universities deny acceptance to students with diagnoses of mental illness. Such students enjoy the protection of the Americans with Disabilities Act (ADA) and should be free from such discrimination. There’s also the more prosaic issue of some students developing mental or emotional disorders while in college. Late adolescence is, for example, a common period in life for the onset of bipolar disorder and schizophrenia. Substance abuse disorders often begin in college, as well.
-Lee Burdette Williams, PhD, is the senior director for mental health initiatives at the National Association of Student Personnel Administrators. This information was included in her article, “Under Pressure: The Growing Demand for Student Mental Health Services” in the May/June 2017 issue of Trusteeship magazine.